Part of Our Ongoing Series Examining Medical Issues Which Affect People in Later Life
Introduction
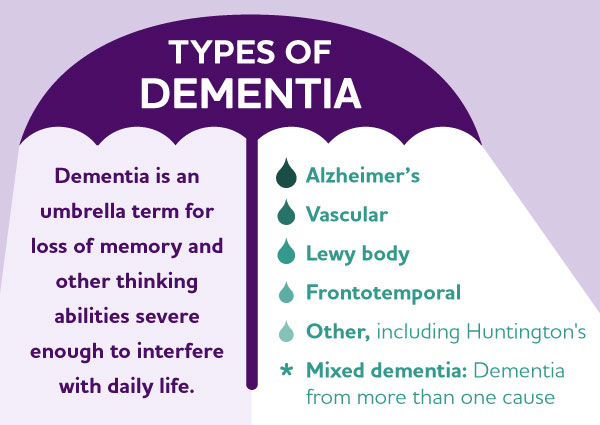
Non-Alzheimer’s dementia — also known as non-Alzheimer’s neurocognitive disorders — encompasses a variety of conditions that cause cognitive decline and memory loss beyond what is considered a normal part of aging. While Alzheimer’s disease is the most common form of dementia, non-Alzheimer’s dementias have different underlying causes and can present with distinct symptoms. These conditions can be challenging to diagnose and manage, as they require a careful understanding of the specific disease process involved.

Image Courtesy of Wellcome Collection Gallery (2018-03-23)
https://wellcomecollection.org/works/zj5vgsbz — CC-BY-4.0
https://commons.wikimedia.org/w/index.php?curid=36013071
Common Varieties
One common type of non-Alzheimer’s dementia is vascular dementia, which occurs when there is a reduced blood flow to the brain, leading to cognitive impairments. Other types include Lewy body dementia, frontotemporal dementia, and mixed dementia, which combines elements of more than one underlying cause.

Courtesy of Wellcome Collection Gallery (2018-03-23) — CC-BY-4.0
https://wellcomecollection.org/works/kr4mtbjs,
https://commons.wikimedia.org/w/index.php?curid=36013065
Risk Factors
Non-Alzheimer’s dementias can affect people of all ages, but they are more commonly seen in older adults, typically after the age of 65. The risk increases with age, and individuals with a history of cardiovascular disease, stroke, or high blood pressure are more susceptible to developing vascular dementia.
Additional risk factors include: lower socio-economic status, inconsistent healthcare access, lifestyle & behavior (smoking, inactivity, poor diet), injuries & illness, and environmental conditions (extreme temperatures, air pollution, poor water quality).
Typical Symptoms
Symptoms of non-Alzheimer’s dementia can vary considerably depending on the specific subtype, but common signs include: memory loss, confusion, difficulty with language or communication, changes in personality and impaired judgment.
In vascular dementia, symptoms may be sudden or progress in a step-wise manner following a series of small strokes. In Lewy body dementia, visual hallucinations, REM sleep behavior disorder and fluctuating cognition are characteristic features. Fronto-temporal dementia often presents with changes in behavior, language difficulties and executive function impairments.
Medical Care
Treatment options for non-Alzheimer’s dementia focus on managing symptoms and addressing underlying causes when possible. Medications may be prescribed to alleviate cognitive symptoms, manage behavioral changes, or improve mood and quality of life. Therapy, both physical and cognitive, can help maintain function and independence for as long as possible. Lifestyle modifications — healthy diet, regular exercise, social engagement — may also play a role in managing the progression of the disease.
Care for Caregivers
In addition to medical interventions, support and resources for caregivers are essential in managing non-Alzheimer’s dementia. Caregiver stress and burnout are common challenges in providing care for individuals with dementia, and access to respite care, support groups, and education can help alleviate the burden on families and improve outcomes for both patients and their loved ones.
So there you have it. Non-Alzheimer’s dementia comprises a diverse group of conditions that share the common feature of cognitive decline beyond normal aging. Understanding the specific subtype of dementia is crucial for appropriate diagnosis and management. While there is currently no cure for most non-Alzheimer’s dementias, early detection, supportive care and a multidisciplinary approach can help improve quality of life for those affected by these challenging conditions.
By Steven Roberts